Table of Contents
EHR software development is the process of designing, building, testing, and deploying electronic health record systems that manage patient data, scheduling, billing, and clinical workflows—compliant with healthcare standards such as FHIR and HL7.
Imagine a time when patient records were stacks of paper, easily lost or damaged in the chaos of a busy hospital.
Luckily, those days are behind us thanks to advanced Electronic Health Record (EHR) solutions. Considered the digital backbone of modern healthcare, EHRs streamline workflows, improve patient care, and save precious time.
And with 88.2% of office-based physicians using EMR/EHR systems, companies that fail to digitize their workflows risk falling behind.
But what do EHR systems do, and how can you integrate innovative EHR software into your healthcare practice?
In this article, we’ll cover the different EHR solution types, the EHR software development process, future trends, and more.
What is an EHR system?
EHR systems are digital platforms that securely store a patient’s complete medical history, replacing traditional paper records. These systems are transforming the way medical data is created, accessed, and managed, empowering healthcare providers with real-time data, enhancing patient care, and paving the way for a more efficient and interconnected healthcare ecosystem.
EMR vs. EHR
While EHR systems aggregate data about a patient’s health over time from various healthcare providers, EMRs (Electronic Medical Records) contain patient data generated within a single healthcare facility.
The graph below identifies the key differences:
|
Feature |
EHR |
EMR |
|
Record Location |
Cloud/Shared |
Clinic-Specific |
|
Data Sharing |
Yes, interoperable |
Limited |
|
Patient Access |
Often available |
Rare |
|
Focus |
Full health history |
Single practice visit |
Here’s a more detailed explanation of the key distinctions between the two:
- Interoperability: EHRs facilitate data sharing among different healthcare systems. On the other hand, EMRs primarily focus on internal data management and may have limited interoperability with external systems.
- Patient engagement: EHR systems empower patients with secure access to their records, appointment scheduling, and direct communication with healthcare providers. EMRs, in contrast, are mainly used by healthcare professionals and provide limited patient access.
- Data analytics: EHRs are equipped with data analysis tools that help healthcare providers make better decisions and improve patient outcomes. EMRs are mainly focused on efficient clinical documentation and in-house workflows, with fewer data analysis capabilities.
Types of EHR Software Systems
EHR systems aren’t one-size-fits-all solutions. They come in various types, each tailored to specific healthcare needs. There are a few main EHR system types based on the:
- Needs they serve
- The tech they use

EHR System Types Based on the Needs They Serve
First, let’s explore the EHR systems based on the needs they serve in the healthcare industry:
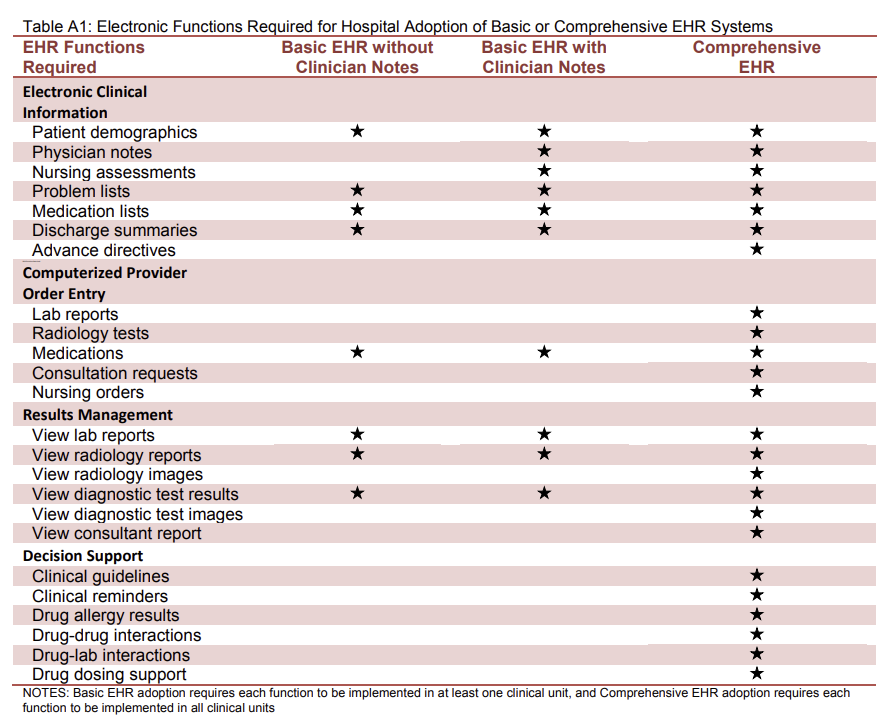
Basic EHR Systems
Basic EHR systems create a centralized hub for patient records, appointments, and billing.
They serve small- to medium-sized healthcare practices, providing cost-effective solutions to replace paper-based records. These systems ensure efficient patient data management and billing processes and represent one of the essential types of healthcare information systems used to streamline clinical and administrative operations.
This type of EHR can simplify administrative tasks and enable quick access to patient histories.
Comprehensive EHR Systems
Comprehensive EHR systems offer an all-encompassing solution that ensures the seamless flow of patient information across multiple departments.
These systems serve the complex administrative needs of bigger organizations, reducing errors through comprehensive data access and enhancing patient care coordination. While basic EHR systems focus on core record-keeping and administrative functions, comprehensive EHRs provide a wider scope of capabilities that help organizations manage operations at scale and support more coordinated care delivery.
Check out the image below from the ONC to better understand the key differences between basic and comprehensive EHR systems:
Specialized EHR Systems
What if your healthcare practice has unique needs? That’s where specialized EHR systems step in, designed specifically for the needs of different medical specialties. Leveraging targeted tools and EHR software features, these systems make it easier to handle specialty-specific patient data and workflows.
For example, an oncology-focused EHR may include tools for tracking treatment plans and outcomes, while a pediatrics-specific system can support growth charts, immunization schedules, and age-based documentation.
Specialized EHRs also provide templates and functions designed for precise documentation, ensuring every unique patient need is met.
Ambulatory EHR Systems
Ambulatory EHR systems assist doctors focused on outpatient care. They’re designed for speed and flexibility, enabling healthcare providers to efficiently track patient data in real time.
Their advantage?
Ambulatory EHR systems automate appointment scheduling, e-prescriptions, billing, and compliance reporting, expediting administrative workflows and contributing to substantial cost savings. They also support informed, on-the-spot clinical decisions while improving patient engagement.
Inpatient EHR Systems
Hospitals are bustling hubs of patient care, and inpatient EHR systems are their backbone. They manage data for admitted patients, ensuring seamless care during their stay.
Inpatient EHRs are built to handle the complex and ever-changing environment of inpatient care. They support care teams with real-time patient data, aiding quick decisions and smoother communication between staff members.
Patient Portals
Patient portals have the potential to enhance doctor-patient relationships, improve health status awareness, and increase adherence to therapy. In other words, they play an important role in improving health outcomes.
This is the core purpose of patient portals, which serve as secure online gateways for patients to access and manage their healthcare data, schedule appointments, and communicate with their care teams. As a result, they boost patient engagement, encourage patients to take an active role in their health, and reduce administrative burdens.

Personal Health Record (PHR) Software
PHR software enables patients to create their health records and maintain their medical histories, appointments, and more.
This type of software grants patients autonomy over their health. It simplifies sharing records with healthcare providers and ensures continuity of care across various settings.

Enterprise EHR Systems
PHR software enables patients to create their health records and maintain their medical histories, appointments, and more.
This type of software grants patients autonomy over their health. It simplifies sharing records with healthcare providers and ensures continuity of care across various settings.

EHR Systems for Telemedicine
EHR systems for telemedicine combine EHR capabilities with telehealth features.
They’re ideal for telehealth providers and practices embracing remote care. These systems empower providers to offer high-quality virtual visits, aided by comprehensive patient data.
By facilitating seamless virtual consultations, they enable providers to access patient records during telehealth appointments, ensuring informed and efficient care. And with over 116 million users of online doctor consultations worldwide in 2024, EHR systems for telemedicine are becoming an essential part of delivering accessible, efficient, and patient-centered remote care.
“Electronic Health Records (EHRs): While not new, advancements in EHR systems have greatly improved patient care. Features like shared records, medication alerts, and seamless provider communication ensure patients receive coordinated, safer care. These tools have made my practice more efficient and patient-focused, allowing me to spend more time addressing individual needs.”
– Dr. Pamela Tambini, Physician & Medical Director at Southeast Detox
EHR System Types Based on the Tech They Use
Here are the EHR system types based on the technology they use.
Cloud-Based EHR Systems
Ever wished you could access patient data from anywhere securely? That’s exactly what cloud-based EHR systems do.
They offer accessibility and flexibility through the cloud and are perfect for healthcare providers looking for data mobility.
Cloud-based EHR systems are gaining more popularity as they enable remote access, reducing geographical limitations and fostering collaboration. They simplify data sharing and backups while ensuring the security and privacy of patient information.
On-Premises EHR Systems
Ever worried about your data residing off-site? On-premises EHR systems keep your data under your roof as they’re hosted locally on your servers.
With on-premises EHRs, you have complete control over data security and compliance, as these systems are known for their robust privacy measures.
Open-source EHR Systems
Want the freedom to customize your EHR? Open-source EHR systems are built on open-source code, allowing users to tweak and tailor them.
They’re suitable for those who seek flexibility and want to avoid vendor lock-in.
What are the benefits?
Open-source EHRs let you shape the software to your unique needs as they offer endless customization possibilities. They’re cost-effective and foster collaboration among developers and users, ensuring ongoing improvements.
EHR Mobile Apps
Ever wanted to check a patient’s record on the go? EHR mobile apps bring EHR systems to your smartphone or tablet, providing access anywhere, anytime.
These apps enhance productivity and patient care, whether you’re at the clinic or in the field, making them perfect for healthcare professionals who need real-time data access.
Key EHR Software Features
EHR systems offer an array of features to streamline care delivery. Let’s explore some of the most essential EHR software features:
- Patient demographics: EHRs store and manage essential patient information, from names and addresses to contact details and insurance data.
- Clinical notes: This feature makes clinical documentation more efficient, as healthcare providers can create and access clinical notes electronically.
- Order entry and management: This feature enables healthcare providers to track orders, monitor patient progress, and prescribe medications, lab tests, and procedures with ease.
- Laboratory and imaging integration: Thanks to their seamless integration with laboratory and imaging systems, EHRs allow healthcare providers to order tests, receive results, and view diagnostic images directly within the system.
- Medication administration: EHR systems support medication administration by providing electronic medication lists, dosage guidance, and allergy alerts. This minimizes medication errors and ensures patients receive the right treatment.
- Billing and claims management: EHR systems can simplify the billing and claims process by generating accurate bills based on provided services and assisting with insurance claims.
- Decision support and analytics: This allows providers to access evidence-based guidelines, drug interaction alerts, and clinical decision support tools.
- Patient portal: Comprehensive EHR systems include patient portals that empower patients to access their records, schedule appointments, and communicate with their providers. This fosters patient-provider collaboration and boosts patient satisfaction.
- AI-powered features: From advanced predictive analytics to automated suggestions and risk scoring, AI helps reduce manual work and improve clinical accuracy. As an AI-forward company, we’ve seen firsthand how these technologies help organizations gain a competitive edge, and we help innovative healthcare providers make AI a key feature of their EHR software. Interested in learning more? Contact us today.
Interoperability
Interoperability is the ability of different applications and systems to communicate, exchange data, and work together effectively. EHR system interoperability ensures the accessibility and usability of patient information across the entire healthcare ecosystem.
Here are a few key interoperability components to be aware of:
- Health Information Exchange (HIE): Health Information Exchange is a critical component of interoperability. HIE enables the secure sharing of patient data among different healthcare organizations, ensuring that your complete medical history is available wherever you seek care.
- Healthcare standards: Some common standards like HL7 (Health Level Seven) and FHIR (Fast Healthcare Interoperability Resources) provide a common language that EHR systems and other healthcare applications understand. This standardized approach ensures that data is not “lost in translation,” making interoperability possible.
- Integration with other systems: Interoperability isn’t limited to sharing patient data alone. EHR systems must seamlessly integrate with other healthcare systems, like practice management systems for billing, PACS for medical imaging, and more. These EHR software integrations ensure that healthcare professionals have a holistic view of patient information at their fingertips.
Quote from an expert:
“PA crucial duty when planning an EHR implementation is assessing the EHR system’s selection criteria and deployment plan with an eye toward interoperability, confidentiality, availability, and integrity of patient health information data, all the while guaranteeing the fast, accurate, and compliant output of reports with regulatory requirements.” says Violet Dsouza.
EHR Software Development Process (Step-by-Step Guide)
EHR system development is a complex process that combines careful planning, cutting-edge technology, and healthcare expertise.
Here’s a breakdown of the step-by-step process:
Initial Requirement Clarification
Before code is written or screens designed, you need to lay the foundation and perform a requirements analysis. At this stage, you should:
- Understand stakeholder requirements: Engaging with stakeholders is crucial to understanding their needs and goals. Here, you can gather insights from clinicians, nurses, administrators, and patients.
- Perform workflow analysis: The EHR system should be tailored to the healthcare workflows of the organization, reflecting their daily operations to enhance efficiency.
- Consider regulatory compliance: EHR systems store and process sensitive patient data. For that reason, a key EHR software requirement is compliance with privacy and security regulations such as GDPR and HIPAA. The HIPAA law is specifically designed to cater to the healthcare industry and guard patient rights.

Initial Rough Project Estimation and Proposal
With the EHR software requirements at hand, it’s time to work on the project estimations and proposal. This includes the following:
- Scope definition: Start by clearly outlining the software’s functionalities and features. For instance, is it a basic EHR system, or does it require complex features and AI capabilities? This forms the project’s roadmap, ensuring every essential element finds its place.
- Resource allocation: Building an EHR system demands the right talents and tools. Carefully select the team members (or development company) with expertise in healthcare software development. Additionally, you should identify the technologies that will be the building blocks of the system.
- Timeline estimation: To maintain a structured workflow, set a tentative schedule for the project. This helps you manage expectations and ensure a smooth development process.
Project Planning Phase
During this phase, you should create a plan for the project with a more detailed timeline and estimates.
At this stage, the EHR system’s blueprints also come to life, and user experience takes center stage.
The design team plans the following:
- System architecture: In this phase, the structural layout of your software is defined. This is the digital framework that ensures all components work harmoniously. Think of it as the architectural plans for a grand building.
- UI design: User-friendliness is paramount in healthcare. It’s important to craft intuitive screens and interactions so the end user can navigate through the system seamlessly.
- Database design: The heart of any EHR system lies in its data. Health data should be stored, retrieved, and managed securely. This ensures that your patients’ information remains confidential and accessible when needed.
Development Phase
The EHR software development phase involves building the digital backbone of your system.
Here, you need to focus on:
- Frontend development: Here, you craft the user interface, ensuring it’s not just visually pleasing but also intuitive. The screens that clinicians, nurses, and administrators will interact with daily are also created on the front end.
- Backend development: This is where the server-side logic, database integrations, and functionalities come to life. Here, you make sure that your EHR system runs seamlessly and securely, handling patient data with utmost care.
- Integration: In the world of healthcare, collaboration is key. Your EHR system must be able to talk to other healthcare systems like PACS, lab systems, or pharmacy systems. This integration ensures a smooth flow of information, making your EHR system an integral part of the healthcare ecosystem.
At this stage, all important milestones are planned.
For each milestone, you need to outline the UI/UX design (which has already been planned for in the previous step) and development.
Interoperability Considerations
At this stage, you make sure the EHR system can seamlessly communicate with other healthcare players. Here it’s important to ensure:
- Standards compliance: You can integrate standards like HL7 and FHIR. These are the common languages that healthcare systems use to exchange information. When your EHR system adheres to these standards, it can fluently converse with other healthcare systems, ensuring that patient data flows without hiccups.
- API (Application Programming Interfaces) development: APIs are like bridges between systems. They allow your EHR to communicate with other healthcare applications, from radiology systems to pharmacy software. By developing robust APIs, you’re ensuring third-party systems can seamlessly interact with your EHR, creating a more comprehensive healthcare ecosystem.
Quality Assurance
Quality assurance is the stage at which every aspect of your system is scrutinized to ensure it performs flawlessly in the high-stakes world of healthcare.
Developers perform various tests, including:
- Unit testing: Here, individual components of your software – from data entry forms to medication history databases – are scrutinized to ensure they work harmoniously without missing a note.
- Integration testing: This confirms that all components of the software work in harmony – the admission module doesn’t clash with the discharge module, and the laboratory data syncs effortlessly with the patient’s record.
- Usability testing: Imagine your software as a tool in the hands of a busy clinician. Usability testing invites actual users to interact with it, ensuring it’s as intuitive as possible. Can a nurse quickly access vital signs? Can a doctor effortlessly update a patient’s history? This testing ensures your EHR system is user-friendly and easy-to-use.
- Compliance testing: In healthcare, adherence to regulations is non-negotiable. Compliance testing ensures your EHR software aligns with industry-specific standards, guaranteeing the confidentiality and security of patient data.
Deployment
Deployment is the pivotal phase where your EHR software moves from development to real-world application.
But before that, your EHR software undergoes a rigorous boot camp in a simulated environment. This controlled testing ground mimics the complexities of actual healthcare settings, allowing for a final shakedown.
After that, it’s time for product rollout.
At this stage, the EHR system is set to join the ranks of healthcare tools and becomes a vital part of actual clinical and administrative workflows.

Training
Now that your EHR software is in place, it’s crucial to ensure that everyone who interacts with it is well-prepared. Training plays a pivotal role in maximizing the benefits of your EHR system.
For this purpose, you need to train those who will directly interact with the EHR system (think: healthcare professionals, administrative staff, and anyone else who’ll use it in their daily tasks).
Training programs are tailored to their specific roles, ensuring they understand how to navigate the software efficiently. From inputting patient data to retrieving critical information, end-user training empowers your team to harness the full potential of the EHR system.
But besides training your end users, you should also provide adequate training for your IT personnel.
Behind the scenes, they are the guardians of your EHR software. They’re responsible for its maintenance, updates, and addressing any technical issues that may arise.
Maintenance & Support
Your journey in EHR software development doesn’t end with deployment. Maintenance and support are ongoing initiatives that ensure your EHR system remains robust, reliable, and responsive to your evolving needs.
Some maintenance and support activities that you need to perform on a regular basis include:
- Regular updates and improvements to keep your EHR system aligned with evolving regulations and user needs.
- Maintaining robust security measures and adhering to data protection laws to safeguard patient data.
- Addressing concerns promptly so healthcare professionals can have a smooth experience at all times.
- Ongoing monitoring to prevent system issues and keep performance optimal.
- Planning for regular data backups and disaster recovery to protect patient data in unforeseen circumstances.
Vetting EHR Software Vendors
Choosing the right EHR software vendor is a pivotal decision in your healthcare organization’s journey.
It impacts how smoothly your operations run, how efficiently you manage patient records, and ultimately, how well you can deliver care.
When navigating this crucial choice, you’ll likely encounter two primary options: off-the-shelf solutions and custom software providers. Let’s explore how to vet both effectively.
Off-the-Shelf Solutions
Off-the-shelf EHR solutions come pre-configured with standard features and functionalities that cater to general healthcare needs.
They are readily available and can be deployed without extensive customization. However, they lack the flexibility of custom solutions, and ensuring they align with your practice’s specific needs is crucial before making a decision.
Here are a few pointers to keep in mind when selecting off-the-shelf EHR software:
- Needs assessment: Start by conducting an in-depth assessment of your organization’s specific needs. Understand your workflows, regulatory obligations, and desired features. Ensure the off-the-shelf solution aligns with these requirements.
- Scalability: Consider the future. Will the solution accommodate your growth? Scalability is vital to avoid outgrowing your EHR system as your practice expands.
- Vendor reputation: Research the vendor’s track record. Look for user reviews, references, and case studies. A reputable vendor should have a history of satisfied customers.
- Training and support: Inquire about the training and support provided. Adequate training ensures your team can utilize the software effectively. Responsive support is essential when issues arise.
Custom Software Providers
Custom software providers specialize in crafting personalized EHR solutions designed to align seamlessly with the unique needs and workflows of individual healthcare organizations.
Opting for a custom EHR software development company is ideal for larger healthcare facilities, hospitals, or practices with specific and complex requirements that may not be adequately met by off-the-shelf EHR systems.
This tailor-made approach ensures that every aspect of your EHR system fits seamlessly into your existing processes, enhancing efficiency and patient care.
Here are a few things to consider when vetting custom software providers:
- Expertise and experience: Look for a team that understands the intricacies of EHR systems and compliance standards. Ensure they have solid expertise not only in development but also in EHR implementation. The company should also showcase substantial experience in the field with similar projects under their belt.
- Customization: One major advantage of custom solutions is the ability to tailor the software to your specific needs. For instance, do you require a system that supports specialized workflows, integrates with existing tools, or incorporates AI-driven features to enhance efficiency and decision-making? Whatever your needs, ensure the provider can accommodate all your specific requirements.
- Security and compliance: Healthcare data security is non-negotiable. Ensure the provider adheres to stringent security practices and compliance standards.
- Project management: Effective project management is crucial. Look for a provider with a well-structured project plan, clear communication channels, and defined milestones.
- Post-launch support: Inquire about the company’s post-launch support and maintenance services. Your EHR system will require updates and ongoing support to remain efficient and secure. So, you should know whether you can rely on the provider to carry out these support activities as well.

Evolving Landscape & Future Trends
The world of healthcare is ever-evolving, and EHR software development is at the forefront of this transformation. To stay ahead in this dynamic landscape, it’s crucial to understand the emerging trends that are shaping the future of EHR systems.
Let’s delve into the exciting developments that are poised to revolutionize healthcare technology.
Mobile Health and EHR on Mobile Devices
Did you know there are over 350,000 health apps available worldwide?
So it should come as no surprise that more and more EHR systems integrate with mobile health solutions.
This allows healthcare professionals to access patient records, update information, and even input data on the go. Patients can also use mobile apps to conveniently view their health records, schedule appointments, and receive real-time updates.
This trend towards mobile health enhances accessibility, promotes patient engagement, and streamlines healthcare delivery.
Artificial Intelligence and Machine Learning in EHR
The rapid development of artificial intelligence and machine learning technologies means they are providing more advanced features than ever before.
Here’s how AI and ML are making a significant impact:
- Clinical decision support: AI-driven algorithms assist healthcare providers in making more informed decisions by analyzing patient data and offering treatment recommendations.
- Predictive analytics: Machine learning models can predict disease outbreaks, patient readmissions, and even individual patient health trends, allowing for proactive care.
- Natural language processing: NLP enables EHR systems to extract valuable information from unstructured data, such as physician notes, improving the accuracy and usefulness of EHR records.
- Automated documentation: AI-powered tools can transcribe voice notes, reducing the administrative burden on healthcare professionals.
Patient Engagement Tools and Remote Patient Monitoring
Patient engagement is a critical factor in healthcare outcomes, and EHR software is increasingly focusing on enhancing this aspect. EHR systems are incorporating patient portals, secure messaging, and telemedicine features to empower individuals in managing their health.
Remote patient monitoring is another trend gaining momentum. Wearable devices and IoT sensors collect real-time health data, which is seamlessly integrated into EHR systems. This allows healthcare providers to monitor patients’ conditions remotely, intervening when necessary and reducing the need for frequent in-person visits.
Conclusion
In the fast-paced world of healthcare, where every second counts, the significance of effective EHR software development cannot be overstated. It’s the cornerstone of a healthcare ecosystem that prioritizes patient care, streamlines processes, and fosters innovation.
As the healthcare industry continues to evolve, you need a reliable partner who can navigate the complexities of EHR software development.
At Scopic, we have nearly 20 years of experience crafting cutting-edge custom software solutions. Our dedicated team of experts understands the unique challenges and opportunities in the healthcare sector—and we leverage the latest AI tools and technologies to deliver EHR software development services that drive greater efficiency and long-term success.
Together, we can harness the power of technology to revolutionize patient care, enhance operational efficiency, and shape the future of healthcare.
Contact us today to learn how we can help you create your custom EHR software.
FAQs About EHR Software Development
What is EHR software development?
EHR software development is the process of planning, designing, and building electronic health record systems that securely store a patient’s complete medical history.
What is the difference between EHR and EMR software?
EHR systems aggregate data about a patient’s health over time from various healthcare providers, while EMRs contain patient data generated within a single healthcare facility.
How long does it take to develop EHR software?
The EHR development timeline depends on the project’s complexity, including the required features, whether it incorporates AI capabilities, necessary integrations, and other technical considerations.
How much does custom EHR software development cost?
The cost of building an EHR system depends on the complexity of the project and the required features. For a tailored quote, contact our team today.
What features are essential in an EHR system?
Key EHR software features include patient demographics, clinical notes, medication administration, billing management, decision support, and AI-powered features that enable greater automation.
What standards should EHR software support?
EHR software should support healthcare data standards such as HL7 and FHIR, along with compliance with privacy and security regulations, including HIPAA and GDPR.
Is EHR software required to be HIPAA-compliant?
Yes, EHR software is required to be HIPAA-compliant to ensure the privacy, security, and proper handling of protected health information.
Can EHR software be customized for different healthcare organizations?
Yes, EHR software can be customized to meet the unique workflows, compliance needs, and EHR software requirements of different healthcare organizations.
Why choose custom EHR software over off-the-shelf solutions?
Custom EHR software is a better choice than off-the-shelf solutions because it can be tailored to specific workflows, compliance needs, integrations, and scalability requirements, providing greater flexibility, efficiency, and long-term value for healthcare organizations.

About Creating EHR Software Development Guide
This guide was authored by Vesselina Lezginov, and reviewed by Mladen Lazic, Chief Technology Officer at Scopic. It has since been updated by Baily Ramsey.
Scopic provides quality and informative content, powered by our deep-rooted expertise in software development. Our team of content writers and experts have great knowledge in the latest software technologies, allowing them to break down even the most complex topics in the field. They also know how to tackle topics from a wide range of industries, capture their essence, and deliver valuable content across all digital platforms.